Retina Eye Services
Macular Degeneration
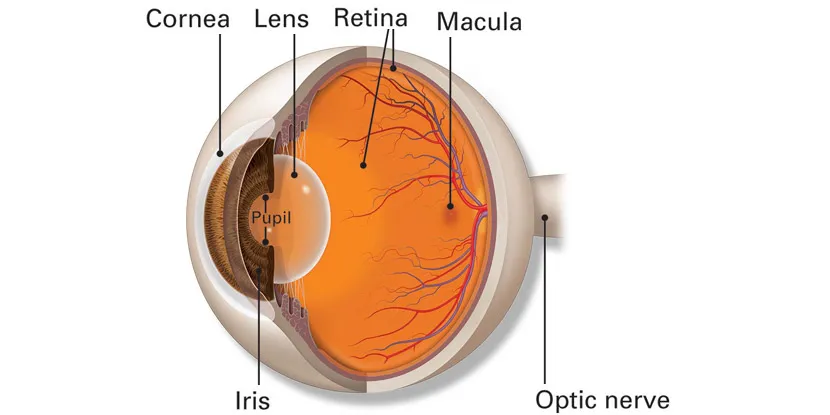
Age-related macular degeneration (AMD) is a common eye disease associated with aging that gradually damages central vision making fine details at distance and up close difficult. Because side vision remains good, macular degeneration doesn’t cause total blindness.
The Progression of AMD can be slow or rapid, but the deterioration of central vision generally occurs over a period of a few years.
So, if you experience the following, call us for a full evaluation:
- Straight lines appear wavy
- Difficulty seeing at a distance
- Decreased ability to distinguish colors
- Inability to see details, such as faces or words in a book
- Dark or empty spots block your center vision
Although it isn’t certain what causes macular degeneration, several studies have shown the following individuals may be at risk:
- Individuals over the age of 60
- People that suffer from hypertension
- Individuals that smoke
- Postmenopausal women
- Individuals with a family history of AMD
Two Types of AMD
Dry AMD
There are two types of macular degeneration, a dry type and a wet type. The Dry form of macular degeneration is more common; about 80% of people with macular degeneration have the dry type. In dry AMD clumps of protein, called drusen, and thinning of the retina can occur causing slow central vision loss. There is no cure for dry macular degeneration. Special eye vitamins called AREDS2, studied by the National Eye Institute, have been shown to slow the risk of progression. T
he AREDS2 vitamins contain a special formulation including:
- Vitamin C (500 mg)
- Vitamin E (400 IU)
- Lutein (10 mg)
- Zeaxanthin (2 mg)
- Zinc (80 mg)
- Copper (2 mg)
After a complete eye exam, we will tell you if vitamins and minerals are recommended for your dry AMD, as not all forms will benefit from the AREDS supplements. Beta carotene should not be used by smokers as it raised the risk of lung cancer.
Wet AMD
Wet macular degeneration is the less common form but more serious. In wet AMD, abnormal blood vessels form and grow under the retina. These vessels can leak fluid, bleed, and cause scarring of the retina causing faster vision loss.
There is no cure for wet AMD but we do have several very effective treatment options to keep patients from losing vision including eye injections and sometimes laser. We will discuss a personalized option best for you and your eyes.
Early detection is your best defense against losing vision. So if you are at risk, schedule an appointment with us for a complete eye exam at least every one to two years. We also recommend you test your vision at home with an Amsler grid.
Test Your Vision with the Amsler Grid
Because AMD can cause a gradual change in vision, you may not notice these changes when they happen. However, the earlier we detect a problem, we can get sight-saving treatment started. Early treatment can help slow or stop further loss of sight. You should use an Amsler grid every day to monitor your vision. One is below for you to use with instructions:
Here is how to use the Amsler grid:
- Keep the Amsler grid in a place where you see it every day. Many people keep an Amsler grid on their refrigerator door or on their bathroom mirror.
- In good light, look at the grid from about 12–15 inches away. Be sure to wear your reading glasses if you normally use them.
- Cover one eye. Look directly at the dot in the center of the grid with your uncovered eye. Notice if any of the lines look bent or wavy. See if any part of the grid looks blurry, dim, or out of shape.
- Now cover your other eye and test your vision this same way again.
Normal Amsler Grid
Call us right away if you notice that any lines or parts of the grid look wavy, blurry, or dim.
Diabetic Eye Disease

What is Diabetes?
Diabetes is a condition that affects the body’s ability to produce and use insulin to control blood sugar (glucose) levels. Diabetes can affect both children and adults. Even if diabetes is well-controlled, it can affect your eyes. The majority of vision loss from diabetes is preventable making early detection key. Yearly eye exam are critical as damage can occur without any symptoms.
What is diabetic eye disease?
Diabetic eye disease includes:
- diabetic retinopathy
- diabetic macular edema
- cataract
- glaucoma
Patients with diabetes are more likely to develop eye problems such as cataracts and glaucoma but the disease’s effect on the retina is the main concern and threat to a person’s vision.
What is Diabetic Retinopathy?
Too much glucose in the bloodstream can cause blood vessel damage throughout the body including in the heart, kidneys, and eyes. The elevated blood sugars can cause damage to blood vessel walls in the retina leading to leaking, swelling, or closing off. Sometimes abnormal new blood vessels grow on the retina. All of these changes can damage vision. Some common symptoms of diabetic retinopathy include blurred vision, often linked to fluctuations in blood sugar levels; fluctuations, floaters, and flashes; or sudden loss of vision. Diabetic patients require routine eye examinations so that related eye problems can be detected and treated as early as possible. Most diabetic patients are frequently examined by an internist or endocrinologist who works closely with the ophthalmologist. A diagnosis of diabetic retinopathy is made following a detailed examination of the retina. Most patients with diabetic retinopathy can be helped if the diagnosis and treatment is early.
The effect of diabetic retinopathy on vision varies widely depending on the stage of the disease. There are two main stages: non-proliferative and proliferative. Non-proliferative daibetic retinopathy (NPDR) is the early stage. With NPDR, tiny blood vessels leak, causing bleeding and/or making the retina swell. When the macula swells, it is called macular edema. This is the most common reason why people with diabetes lose their vision.
Also with NPDR, blood vessels in the retina can close off. This is called macular ischemia. When that happens, blood cannot reach the macula. Sometimes tiny particles called exudates can form in the retina. These can affect your vision too.
Proliferative diabetic retinopathy (PDR) is the more advanced stage. In this stage, circulation problems cause areas of the retina to become oxygen deprived. New, very fragile blood vessels begin to grow and develop into places they shouldn’t be. This process is called neovascularization. Unfortunately, these delicate vessels leak and hemorrhage quite easily causing hemorrhages into the vitreous gel of the eye and can cause associated decreased vision. Extensive proliferative retinopathy can lead to other serious problems such as retinal detachment.
These new blood vessels can form scar tissue. Scar tissue can cause problems with the macula or lead to a detached retina.
PDR is very serious, and can steal both your central and peripheral (side) vision.
Over time diabetes affects the circulatory system of the retina with the earliest phase of the disease termed background or non-proliferative diabetic retinopathy. In this phase of diabetic retinopathy, arteries in the retina become weakened, may close off, and/or may leak blood, lipid, and fluid with associated decreased vision.
These new blood vessels can form scar tissue. Scar tissue can cause problems with the macula or lead to a detached retina.
PDR is very serious, and can steal both your central and peripheral (side) vision.
Over time diabetes affects the circulatory system of the retina with the earliest phase of the disease termed background or non-proliferative diabetic retinopathy. In this phase of diabetic retinopathy, arteries in the retina become weakened, may close off, and/or may leak blood, lipid, and fluid with associated decreased vision.
What is Diabetic Macular Edema?
Macular edema happens when fluid builds up on the retina and causes swelling and blurry vision. Diabetes can cause macular edema. Diabetic macular edema can lead to permanent vision loss.
Diabetes and cataracts
Elevated blood sugar from diabetes can causes cataracts. Patients with diabetes may develop cataracts earlier than non-diabetic patients. Special considerations for surgery may be required depending on the extend of diabetic eye disease. You may need cataract surgery to remove lenses that are clouded by the effects of diabetes. Dr. Patel is both a cataract surgeon and a fellowship-trained retina specialist. She will develop a customized plan for your eye.
Diabetes and glaucoma
Glaucoma is a group of diseases that cause damage to your eye’s optic nerve. This damage leads to irreversible loss of vision. Having diabetes doubles your chance of getting glaucoma.
What Other Eye Problems Are Related to Diabetes?
Diabetes can cause vision problems even if you do not have a form of diabetic eye disease.
These can include:
- Blurry vision. If your blood sugar levels change quickly, it can affect the shape of your eye’s lens, causing blurry vision. Your vision goes back to normal after your blood sugar stabilizes. Have your blood sugar controlled and stable for at least 1 week before getting your eyeglasses prescription checked. This ensures you receive the best prescription.
- Double vision. Diabetes can damage the nerves that move the eyes and help them work together. This nerve damage can lead to difficulty moving the eyes and double vision.
Diabetes is a risk factor for several other eye diseases. They including:
How Do We Diagnose Diabetic Eye Disease?

Optical Coherence Tomography (OCT)
A complete eye exam with dilation of the pupils is needed to assess and diagnose diabetic retinopathy. This allows Dr. Patel to look through a special lens to see the inside of your eye best. If needed, we may combine the eye exam with diagnostic testing with the most advanced technology including optical coherence tomography (OCT) to look more closely at the retina. We use swept-source technology to obtain detailed images of the different layers of the retina and calculate its thickness from visit to visit.
Fluorescein Angiography
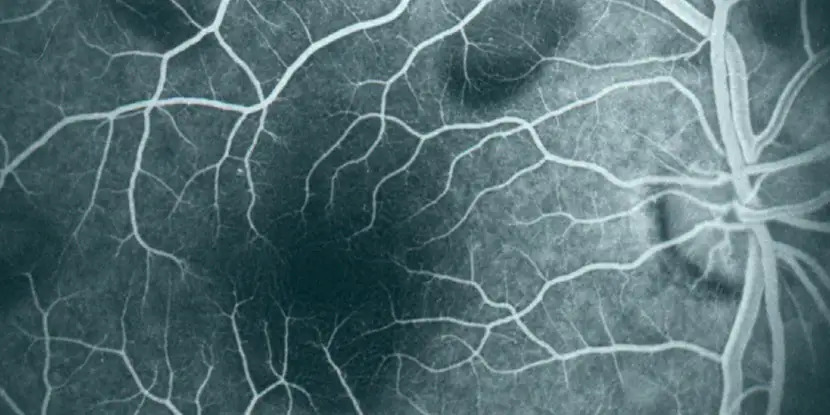
Sometimes we may use, Fluorescein angiography to see what is happening with the blood vessels in your retina. Fluorescein angiography uses a yellow dye called fluorescein, which is injected into a vein (usually in your arm). The dye travels through your blood vessels. A special high-definition camera takes photos of the retina as the dye travels throughout its blood vessels. This shows if any blood vessels are blocked or leaking fluid. It also shows if any abnormal blood vessels are growing.
What Treatments are Available for Diabetic Retinopathy?
The treatment of diabetic retinopathy is based on the extent of damage and the status of your eyes. Often, different treatment options are used such as intravitreal injection or laser. Dr. Patel will develop a personalized plan for your treatment based on the latest science and adjust based on your individual response.
Sometimes a surgery, called vitrectomy, is needed for advanced proliferative diabetic retinopathy. In this procedure, the vitreous gel and blood from leaking vessels in the back of your eye is removed. This allows light rays to focus properly on the retina again. Scar tissue also might be removed from the retina.
5 Ways to Prevent Vision Loss from Diabetic Retinopathy
- If you have diabetes, talk with your primary care doctor about controlling your blood sugar. High blood sugar damages retinal blood vessels. That causes vision loss.
- Do you have high blood pressure or kidney problems? Ask your doctor about ways to manage and treat these problems.
- See your ophthalmologist regularly for dilated eye exams. Diabetic retinopathy may be found before you even notice any vision problems.
- If you notice vision changes in one or both eyes, call your ophthalmologist right away.
- Get treatment for diabetic retinopathy as soon as possible. This is the best way to prevent vision loss.
Retinal Tears and Detachments
Retinal detachments are the separation of the retinal tissue from the inside wall of the eye. Similar to wallpaper coming loose from the wall, the retinal tissue may develop folds or come completely away from its proper position along the interior of the eye resulting in loss of vision.
Retinal tears involve a rip or tear in the tissue compromising the retina. They usually arise from a thinning or degenerative change in the peripheral retina. The retina is a layer of photoreceptor nerve cells lining the back of the eye and just like film in a camera, the retina reacts to the presence of light. These photoreceptor nerve cells generate an electrical impulse whenever they are exposed to light and these nerve impulses travel through the optic nerve to the brain where an image is perceived.
When the retina is torn, vitreous fluid (the inner gel fluid of the eye) is able to seep through the tear and accumulate behind the retina. This causes the retina to detach from the inside lining of the eye. Once a retinal detachment is started, it usually continues until most of the retina is completely separated from the interior of the eye resulting in blindness in the effected region.

Who Is at Risk for a Retinal Detachment?
You are more likely to have a detached retina if you:
- need glasses to see far away (are nearsighted)
- have had cataract, glaucoma, or other eye surgery
- take glaucoma medications that make the pupil small (like pilocarpine)
- had a serious eye injury
- had a retinal tear or detachment in your other eye
- have family members who had retinal detachment
- have weak areas in your retina (seen by an eye doctor during an exam)
What are the Symptoms of Retinal Tear or Detachment?
A detached retina should be examined by an ophthalmologist right away. Otherwise, you could have permanent loss of vision.
Call an ophthalmologist immediately if you have any of these symptoms:
- Seeing flashing lights all of a sudden. Some people say this is like seeing stars after being hit in the eye.
- Noticing many new floaters at once. These can look like specks, lines or cobwebs in your field of vision.
- A shadow appearing in your peripheral (side) vision.
- A gray curtain covering part of your field of vision.
Symptoms of retinal tears and detachments are new floaters, the sudden appearance of flashes of light in the vision, or a noted new occurrence of a shadow or curtain being pulled over a portion of the vision of one eye. Also, sudden decreased vision can be a symptom of a retinal tear or detachment.
Treatment options include laser, pneumatic retinopexy, and surgery. Advances in surgical technology and techniques have resulted in a good success rate for repairs of retinal tears and detachments. The success of these surgical procedures is related to the size of the tear and the amount of detachment as well as the timeliness of the treatment.
Flashes and Floaters
Flashes and floaters can be a common visual for many people. Flashes and floaters all happen in what is called vitreous humor. The vitreous is the clear gel-like substance between the lens and the retina. As you age, your vitreous humor shrinks, and the proteins that are inside of that gel essentially start looking like little floating objects inside of your eye. You don’t actually see the protein itself, rather the shadow from the protein gets passed through.
Are Flashes and Floaters Serious?
Most of the time, flashes and floaters can be a natural occurrence without the threat of any serious vision loss. Although, the sudden onset of flashes and floaters with other symptoms such as shooting pain, or a rapid decline in vision can signal a more serious condition such as retinal detachment.
What Can I Do To Prevent Flashes and Floaters?
If your flashes and floaters don’t naturally disappear over a couple of weeks there are procedures that treat these retina conditions. If the sudden onset of flashers and floaters could lead to permanent vision loss your retina specialist will consider vitrectomy surgery if needed.
Scheduling a yearly eye exam is crucial in treating potentially harmful flashes and floaters. The sudden onset of flashes and floaters symptoms may be scary but our team of ophthalmologists are here to help you.