Uveitis occurs when the middle layer of the eyeball gets inflamed (red and swollen). This layer, called the uvea, has many blood vessels that nourish the eye. Uveitis can damage vital eye tissue, leading to permanent vision loss. Eye inflammation can occur due to an infection or chronic disease, such as uveitis, juvenile idiopathic arthritis, ankylosing spondylitis, and rheumatoid arthritis. Uveitis is a leading cause of blindness in the United States. Dr. Patel is a fellowship-trained, nationally recognized uveitis specialist with years of experience treating patients with all types of uveitis.
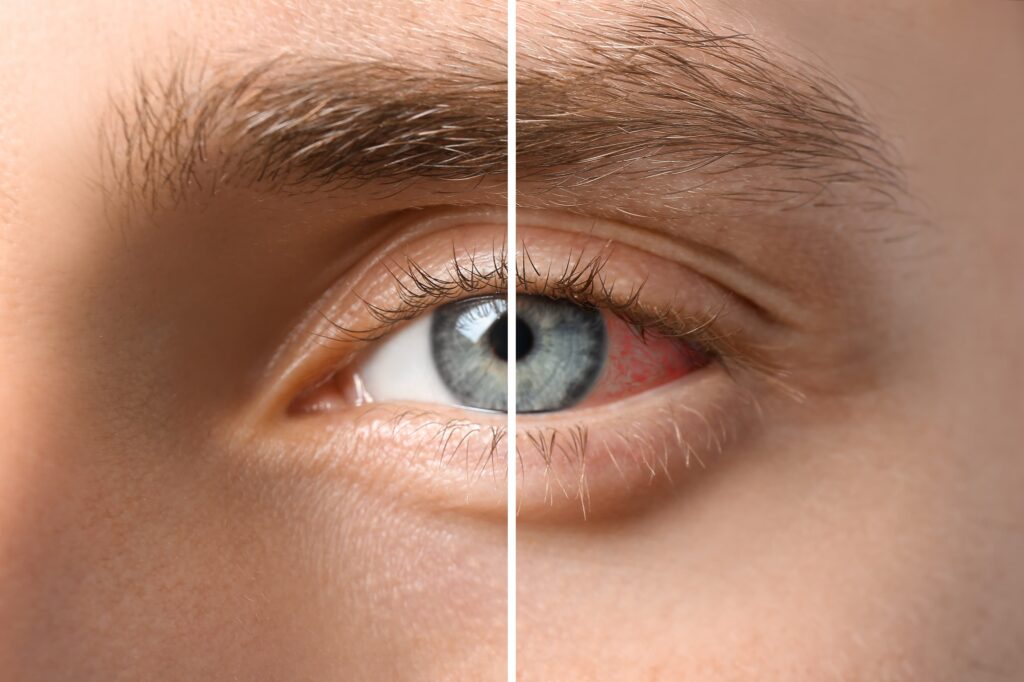
There are 3 types of uveitis. They are based on which part of the uvea is affected. Inflammation of the uvea near the front of the eye is called anterior uveitis. It can start suddenly and symptoms can last many weeks. Some forms of anterior uveitis are ongoing, while others go away but keep coming back.
Inflammation of the uvea in the middle of the eye is called intermediate uveitis. Symptoms can last for a few weeks to many years. This form can go through cycles of getting better, then getting worse. Inflammation of the uvea toward the back of the eye is called posterior uveitis. Symptoms can develop gradually and last for many years. In severe cases, all layers may be involved.
It’s important to watch for signs of eye inflammation. Symptoms often include:
If you experience symptoms of eye inflammation or vision changes, call Dr. Patel and her team for an eye exam as soon as possible to help prevent permanent vision loss.
The cause of uveitis and other forms of eye inflammation isn’t always clear, but genetics may play a role. You are more likely to get uveitis if you have or have had:
When left untreated, inflammation may lead to cataracts, glaucoma, optic nerve damage, retinal detachment, or permanent vision loss.
Dr. Patel will examine the inside of your eye to determine whether you have signs of present or past inflammation. Using our advanced diagnostic equipment, she will identify what areas of the eye are involved. Since uveitis is often connected with other diseases or conditions, some tests may be needed. They may include a physical exam, blood or skin tests, examination of eye fluids, and imaging tests, such as X-rays. Dr. Patel will ask about other diseases or health problems you have had.
Uveitis needs to be treated right away to prevent lasting problems. Dr. Patel often treats uveitis with eyedrop medicine that reduces inflammation, often corticosteroids. They may also use an eye drop to widen (dilate) the pupil, which helps reduce pain and swelling. Sometimes antibiotics are used as well. She might suggest you avoid wearing contact lenses for a period of time until your eyes heal. In some cases, Dr. Patel may recommend injections (shots) or pills. Dr. Patel may also collaborate with other experienced specialists, such as rheumatologists, infectious disease specialists, or pulmonologists.
If you have cataracts, glaucoma, or vision loss, Dr. Patel might also recommend eye surgery to treat your specific eye disease. Seeking treatment early before serious complications arise can help save your vision.
Don’t live with eye inflammation when it could be a sign of a serious eye disease requiring treatment. Schedule an appointment with ORA Vision.
Adapted from geteyesmart.com by the American Academy of Ophthalmology